Depression is different than feeling sad or down. It is a medical condition affecting the way mood is controlled by the brain. Someone with Depression can’t just “snap out of it.” Depression affects the way he or she thinks, feels and acts. It becomes a negative lens through which he or she sees and experiences the world.
When Depression happens, it often lasts for many months and then sometimes gets better. This is called an episode of Depression. Most people who get Depression will experience many episodes during their lifetime. Depression is often called Major Depressive Disorder (MDD).
Sometimes a negative event (such as the loss of a loved one, or severe and prolonged stress) will trigger an episode of Depression but often episodes will occur spontaneously. Depression is not caused by the usual stresses of life. Depression is often accompanied by feelings of anxiety and causes significant problems with family, friends, work or school.
Depression, and other mental disorders, should only be diagnosed by a medical doctor, clinical psychologist, or a trained health provider who has spent time with the teenager and has conducted a proper mental health assessment. Diagnoses are complicated with many nuances. Please do not attempt to diagnose someone based on the symptoms you read about in magazines or on the internet. If you are concerned, speak to a trained health professional.
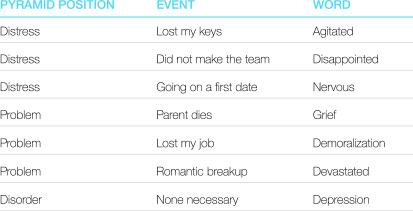
It can be confusing when people use the word “depression” to mean different things. We should try to save the word “depression” to mean the mental disorder of Depression, and use other, more exact words to describe the negative emotions that we feel.
Use the Right Words!
Major Depressive Disorder (MDD)
Someone with MDD will experience episodes of intense depression (lasting weeks to years), separated by periods of relatively stable mood. When people refer to Depression, they usually mean MDD.
Persistent Depressive Disorder (formerly Dysthymia)
People with Persistent Depressive Disorder will experience depressive episodes that are less intense than in MDD but last much longer. For teenagers, these depressive episodes last at least one year and for adults, they last two years or more
Disruptive Mood Dysregulation Disorder
Children up to 18-years-old can be diagnosed with Disruptive Mood Dysregulation Disorder if they have persistent irritability and frequent episodes of unreasonable verbal and physical aggression.
To determine if someone you care about may be at risk for Depression, consider the following questions:
- Does the person feel sad or low most of the time?
- Has the person lost interest in activities he or she usually enjoys?
- Does he or she have trouble concentrating?
- Does he or she feel fatigued or tired much of the time?
- Does he or she feel hopeless or worthless?
- Does he or she experience much less enjoyment in life?
- Has this behaviour lasted at least two weeks, and been present every day for most of the day?
There are three areas of symptoms that often present in youth experiencing depressive episodes. Here are some things to watch for:
Mood
- Feeling persistently depressed, sad, unhappy or something similar
- Feeling a loss of pleasure, or a noticeable disinterest in all or almost all activities
- Feelings of worthlessness, hopelessness or excessive and inappropriate guilt
Thinking
- Diminished ability to think, concentrate or make decisions
- Suicidal thoughts/plans or preoccupation with death and dying
Body Sensations
- Excessive fatigue or loss of energy
- Significant sleep problems (difficulty falling asleep or sleeping excessively)
- Physical slowness or, in some cases, restlessness
- Significant decrease or increase in appetite that may lead to noticeable weight change
If someone in your life has five of the above symptoms (with at least one of them being a mood symptom) present every day for most of the day during the same two week period, then he or she may be experiencing Clinical Depression (MDD). Talk to your family doctor about your concerns. This behaviour cannot be due to a substance, medicine or another illness and must be different than the individual’s usual mood state.
*In accordance with the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition.
Remember, you cannot diagnose someone with Depression without a proper mental health assessment conducted by a properly trained health provider.
http://teenmentalhealth.org/learn/mental-disorders/depression/